Customizing MOD-59 and other Insurer-Specific Rules with Your Physical Therapy Billing Software
When dealing with the confusing realm of modifiers for medical billing, it’s critical to have physical therapy billing software that is fully customizable, to maximize payments on your claims. That’s why ClinicSource offers you the ability to create custom modifier rules that are specific to each insurer. Let’s take a look, using the complicated CPT Code Billing Modifier 59 as an example.
Modifier 59
If you’re sometimes confused about when to use modifier 59, then you are not alone. At times, it may be necessary to indicate that a procedure or service was distinct or independent from other non-Evaluation and Management services (E/M) performed on the same day.
Modifier 59 is used to identify procedures/services, other than E/M services, that are not normally reported together but are appropriate. Therapy documentation software must support a different session, different procedure, and different site or separate injury. However, when another already-established modifier is appropriate, it should be used rather than billing modifier 59.
Please keep the following key points in mind when applying CPT Code Billing Modifier 59:
- Use modifier 59 to identify a procedure that is independent from the other non E/M services that the provider performs on the same day.
- Modifier 59 applies to procedures or services not typically reported together, but are appropriate in a specific situation.
- Modifier 59 tells the payer that the provider does not ordinarily perform the procedure with another procedure for the same patient on the same day by the same provider.
- Do not append modifier 59 to the E/M service.
Again, in order to report CPT Code Billing Modifier 59, the provider’s documentation must support a:
- Different encounter or session
- Different surgery or procedure
- Different organ system or body site
- Separate incision or excision
- Separate lesion
- Separate Injury
Example: 92523 (Evaluation of speech sound production) payable with 96125 (Standardized Cognitive Performance Testing) with mod 59.
Unfortunately, not all insurers will pay you for billing modifier 59 even if you code in compliance with CPT rules. Be sure to appeal any denied or bundled claims. A review of your documentation by the insurer may actually result in payment for your work.
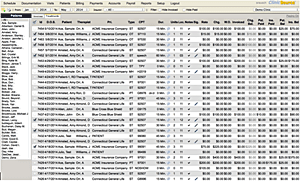
How To Create Custom Billing Modifier Rules with ClinicSource
To create a rule in ClinicSource, simply go to Setup > Insurers and select the insurer from the column to the left that requires the modifier. Scroll down on the main window (under the Default Rates section) and you will see Modifiers. Select the discipline in the drop down selection box, then click on the button to the left of the discipline once selected.
The rule box will open below. Select the Non E/M CPT Code, set the appropriate Diagnosis (most commonly set to all), type in the Modifier (in this case modifier 59), set the rule to Multiple Procedures, enter a Rate and Allowed amount and save.
When an E/M code and Non E/M code are selected and saved in the same Visit, ClinicSource will apply the 59 Modifier to the Non E/M code when invoicing.
Don’t Already Use ClinicSource? Try It for Free
If you’re not already taking advantage of this powerful, easy-to-use therapy EMR and billing system, try ClinicSource for free, with absolutely no obligation. Or request a free live demo from one of our system experts.
Let Us Show You