Highlights
- SOAP notes are critical for tracking patient progress, but upkeep as the client progresses can be tedious.
- Techniques to improve your note taking skills can streamline the process.
- Therapy notes software allows you to create templates for taking notes so they’re easier to maintain and read.
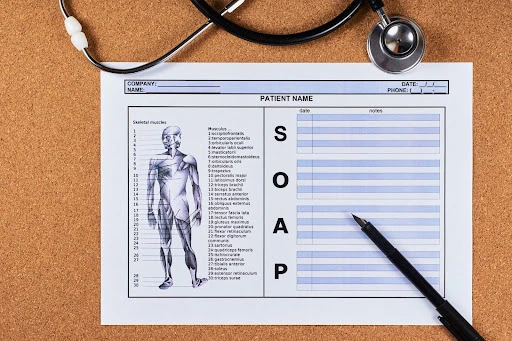
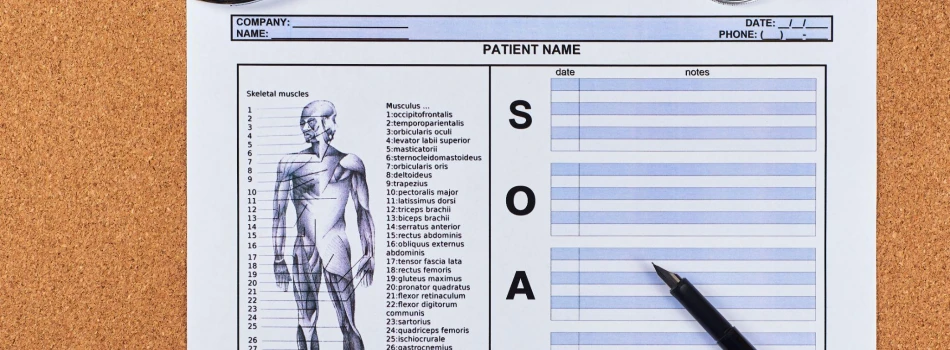
SOAP (Subjective, Objective, Assessment, Plan) notes are an essential component of providing care and treatment for patients. It’s vital to document data and information from every patient encounter. Therapy SOAP notes monitor and document patient progress, log services, and communicate patient information to other professionals.
While it can be overwhelming to take notes for a high volume of daily patients, reviewing the following tips and using therapy notes software makes it easier to implement a seamless process for your practice.
SOAP Notes Overview
SOAP notes were first introduced by Dr. Lawrence Weed about 50 years ago. Their creation revolutionized the medical industry as the first proper method of documentation. The exercise varies by field and allows plenty of room for customization, but there are four universal components.
Subjective
The subjective section is for patient input. These are statements provided by the patient about their symptoms and current condition. Some healthcare professionals rely on another acronym for proper subjective documentation. The most common is “OLD CARTS.”
- O – Onset – when the condition started
- L – Location – where the condition is located
- D – Duration – how long the patient has had the condition
- C – Character – description of the condition
- A – Alleviating/aggravating factors – what makes the condition better or worse
- R – Radiation – whether the condition moves or stays stationary
- T – Temporal pattern – whether the condition is worse during a specific time of day
- S – Severity – Rating of the pain on a scale of 1-10
Objective
The objective section is about measurable results and quantitative data. All statements under objective should include supporting data. Record the conclusions about this data separately.
Assessment
The assessment section is an analysis of the subjective and objective results. Make unbiased, data-driven decisions by reviewing the subjective and objective sections separately. Reviewing the assessment section from previous visits is an ideal way to track progress and make sure details are not lost over time.
Plan
The plan section is about treatment and rationale. This includes the next steps for the patient, take-home assignments, and anticipated agenda for the next session.
Tips for Writing SOAP Notes
Here are some quick tips for writing effective SOAP notes that won’t take time away from one-on-one time with patients.
1. Think about the purpose of the note
The tedious nature of SOAP notes can overshadow their importance. In addition to communicating patient information and progression to other professionals, SOAP notes serve a variety of purposes:
- Ensuring proper billing from insurance companies
- Providing rationale for ongoing services
- Creating a consistent and effective method of treatment for every patient
- Offering a balance between patient input and clinician guidance
ClinicSource templates provide a consistent format for documentation tailored to the treatment provided. The result is a cohesive and well-structured SOAP note every time.
These templates make it easier for you to find the appropriate time to write cohesive notes and create a space for you to keep it professional and accurate without being biased or judgemental.
2. Complete notes within a reasonable time frame
Complete notes as soon as possible following treatment sessions. Completing notes in a timely fashion means more accuracy, and falling behind on documentation can delay insurance reimbursement.
ClinicSource templates pre-populate basic patient information, allowing clinicians to spend less time typing repetitive information and more time documenting session specifics. The time savings means more quality time with patients, which benefits patients and your practice’s bottom line.
3. Double-check key details within your SOAP note
Align the details of your SOAP note templates. Double (or triple) check these crucial details:
- Be sure the start time, end time, and units billed match the session length.
- Make sure that all CPT codes match up with the billing statement.
- Be certain that patient names and diagnosis codes are accurate throughout.
By using ClinicSource templates, accurate information flows automatically from section to section, reducing the chances of clerical errors.
4. Be mindful of meaningful goals and objectives
SMART (specific, measurable, attainable, relevant, and timely) goals keep SOAP notes effective and consistent over time. SMART goals ensure that all parties (patient, parents, insurance companies, physicians, etc.) understand the mission of your work.
In a ClinicSource SOAP note template, goals and objectives from a patient’s treatment plan automatically populate in the Objective portion of the note, making it easy for clinicians to enter specific data points and track progress.
5. Compare patient performance across sessions
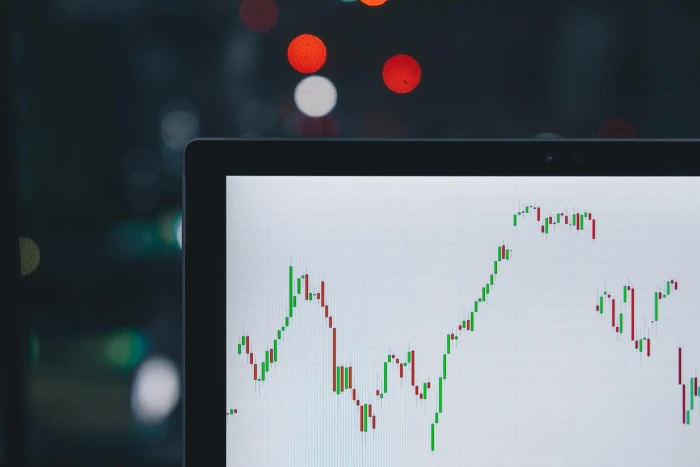
A lone data point is not useful. However, when viewed next to previous data, it illustrates patient progress or setbacks.
ClinicSource SOAP notes make it easy to add a comment about data trends to the Assessment portion of the note. In this section, be sure to analyze and interpret your data, especially as it relates to a patient’s performance. Clinicians can generate a Progress Summary Note, which instantly graphs data from a selected time frame.
6. Don’t underestimate home education programs
Make sure to document home education and carryover programs in SOAP notes. This is an important exercise for patients to practice their developing skills. Additionally, insurance companies often make this a requirement for billing.
Document all recommended strategies and interventions with directions on home implementation.
Final Thoughts
By following these simple tips, you can ensure that your SOAP notes are effective and meet the needs of all involved parties. Keep in mind that SOAP notes are a living document; they should be updated as a patient’s condition changes.
ClinicSource offers customizable SOAP note templates to make documentation easier than ever. Book a demo today to see how our easy-to-use platform helps you create SOAP notes that are tailored to your specific needs, giving you more time to focus on what matters most – providing quality patient care.
Let Us Show You